Recently, the HARMONi‑6 study, led by Professor Lu Shun, academic leader of the Department of Oncology at Shanghai Chest Hospital, affiliated hospital of Jiao Tong University School of Medicine, and Director of the Shanghai Lung Tumor Clinical Medical Center, achieved a breakthrough. On October 19, the results were published in the high-impact international journal The Lancet, and on the same day, the study was presented as a Late-Breaking Abstract (LBA) at the ESMO Congress 2025 by Professor Lu.
The study investigated the efficacy and safety of a globally novel “tumor immunotherapy + anti-angiogenesis” bispecific antibody, Ivonescimab, combined with chemotherapy as a first-line treatment for advanced squamous non–small cell lung cancer (NSCLC), thereby establishing a new paradigm for treating advanced squamous lung cancer. Professor Lu served as the corresponding author of the publication, and Dr. Chen Zhiwei, Deputy Director of Oncology at the Shanghai Chest Hospital, was the first author.
01 Breaking the Bottleneck: Upgrading Treatment for Squamous Lung Cancer
Professor Lu Shun Presents HARMONi‑6 Study Results at the ESMO Congress 2025
Squamous cell lung cancer accounts for approximately 35% of all NSCLC, and around 70% of patients are diagnosed at an advanced stage. Traditional chemotherapy offers limited efficacy, with a 5-year survival rate of less than 10%, and the overall prognosis remains poor. With the development of immunotherapy, PD–1 inhibitor–based combination chemotherapy has become a widely recognized standard of care in first-line treatment. However, this treatment approach still faces significant unresolved clinical challenges: patient survival has plateaued, and anti-angiogenic agents cannot be widely applied due to bleeding risks. Consequently, there is an urgent clinical need for more breakthrough first-line treatment strategies that can simultaneously optimize both efficacy and safety.
Ivonescimab is a domestically developed PD-1/VEGF bispecific immunotherapy for the treatment of cancer. Compared with traditional immunotherapies, it not only exerts anti-tumor effects but also avoids the bleeding risks associated with anti-angiogenic agents. To further evaluate the clinical efficacy of Ivonescimab combined with chemotherapy, Professor Lu and his team initiated the Phase III clinical trial “HARMONi‑6: Exploring the Efficacy and Safety of PD-1/VEGF Bispecific Antibody Ivonescimab Plus Chemotherapy versus Tislelizumab Plus Chemotherapy as First-Line Treatment for Advanced Squamous Non–Small Cell Lung Cancer.”
02 “Dual-Antibody” Regimen: Enhanced Efficacy and Safety for Patients

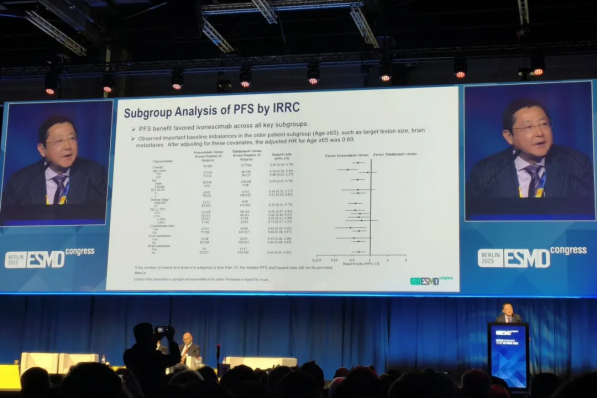
The study enrolled a total of 532 patients, who were randomly assigned to receive either Ivonescimab plus chemotherapy or tislelizumab plus chemotherapy. The results demonstrated that the median progression-free survival (PFS) in the Ivonescimab group was 11.14 months, compared with only 6.9 months in the tislelizumab group. In terms of safety,the Ivonescimab group also performed exceptionally well, showing similar outcomes to the control group, with serious bleeding occurring in only 1.9% of patients. This breakthrough effectively overcomes the longstanding issue of high bleeding risk associated with anti-angiogenic drugs in squamous lung cancer treatment.
These findings confirm that Ivonescimab therapy achieves the most prolonged first-line PFS historically reported for advanced squamous NSCLC, significantly extending patient survival and simultaneously enhancing both efficacy and safety. Furthermore, this treatment strategy fills a critical gap in the application of anti-angiogenic agents for squamous NSCLC, representing a major advancement in the field.
Based on these outstanding results, the marketing application for the new indication of Ivonescimab plus chemotherapy as a first-line treatment for advanced squamous NSCLC is currently under review, offering new hope for patients with advanced disease that may surpass existing standard-of-care options.
03 Three Decades of Dedication: Professor Lu as a Global Leader in Lung Cancer Research

Professor Lu has dedicated over 30 years to precision treatment and research in lung cancer, establishing himself as a leading scholar in the field and serving as principal investigator for multiple national key projects. He led the LAURA study, which established the global Phase III standard for the diagnosis and treatment of EGFR-mutant lung cancer. The results were published in the top-tier international journal The New England Journal of Medicine, demonstrating the global impact of his research.
He pioneered perioperative immunotherapy strategies and targeted resistance-reversal approaches, breaking through longstanding barriers to the cure of lung cancer. Several of his“China-originated” protocols have been incorporated into international guidelines, and his findings have been published in top journals such as JAMA, reflecting his leadership at the forefront of the discipline.
In recent years, Professor Lu has spearheaded 28 domestic and international lung cancer indication studies, including 17 Class 1.1 new drugs in China, facilitating the market approval of numerous domestically developed drugs and their gradual inclusion in national insurance coverage. He has also promoted the overseas approval of domestically produced drugs in countries including the UK and Japan, benefiting over one million patients worldwide.
The newly published study further enhances the clinical benefits of first-line therapy for non–small cell lung cancer, offering advanced squamous NSCLC patients a novel immunotherapy plus anti-angiogenesis combination regimen. Professor Lu emphasizes that this study not only represents a significant advance in NSCLC treatment but also constitutes a breakthrough in global tumor immunotherapy, with the potential to reshape the global oncology landscape through a“China-originated” approach.

